The Center for Connected Health Policy released the Spring 2022 Report on State Telemedicine Law and Medicaid Program Policy in May. In particular, this document tracks changes in the state’s Medicaid policy since the fall of 2021.
The situation is about the same, but these advances represent significant advances in the expansion of telemedicine access across the United States.
With the advent of the COVID-19 pandemic, many states have adopted temporary telemedicine regulations to address difficult situations. These advances have made health care accessible to millions of Americans. Since the fall of 2021, many of these policies have been permanent changes.
This article explains telemedicine as a concept and why it is important, focuses on recent changes in the law on Medicaid reimbursement, and suggests ways to further expand.
Definition of telemedicine
Telehealth uses electronic information and telecommunications technology to provide healthcare to patients in a physical location that is different from the healthcare provider. However, the state builds its legal definition differently by allowing some modality to redeem Medicaid and not others.
According to the report, all 50 states and the District of Columbia are reimbursing providers for some form of live video service. Other forms of telemedicine, such as store-and-forward, remote patient monitoring (RPM), and voice-only services, have less institutional support.
Store-and-forward services allow patients to send health information electronically. This information will be confirmed by the provider later. Twenty-five states limit this modality by providing “real-time” health care to be eligible for Medicaid reimbursement.
RPM uses new technology that allows practitioners to monitor patients without visiting them directly. RPM is allowed to some extent in 30 states, but many states offer only Medicaid refunds to home care providers, limit the clinical status that can be monitored, limit the type of information that providers can collect, and so on. It imposes restrictions on the use of RPM.
Voice-only (telephone) services have not traditionally been the accepted modality for the redemption of the state Medicaid. However, because many Americans lack the high-speed broadband internet needed to engage in video calls, the state has increasingly allowed these services during the COVID-19 pandemic. Currently, 29 state Medicaid programs offer some form of refund, but often only for specific disciplines or services.
Why redemption is important
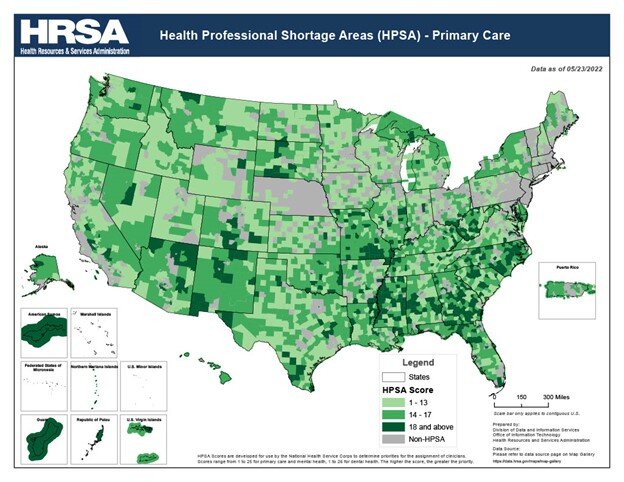
Why do we need to worry about whether the state Medicaid policy will refund telemedicine services? As the map above shows, many parts of the country (especially rural areas) lack medical professionals. The lack of specialists in these areas can be particularly problematic for individuals with chronic illnesses.
Telemedicine and related technologies allow individuals in these regions to receive treatment from healthcare providers in other parts of the state or country. Telemedicine can also accelerate treatment time. If local health care providers are experiencing staff shortages, telemedicine represents a way for residents to receive care without having to wait weeks for appointments.
Finally, increased access to preventive care through telemedicine reduces the need for expensive emergency room visits.
Since the fall 2021 CCHP report, several states have updated their permanent policies on telemedicine. The new private payer law has not been enforced, but some states have changed their policies regarding the reimbursement of telemedicine Medicaid. Some of these changes are related to the modality of care.
Iowa, Massachusetts, and South Dakota have all added store-and-forward to the legal definition of telemedicine for Medicade reimbursement. In Virginia and Wisconsin, patients are now eligible for a Medicaid refund for RPM services (although there are some eligible conditions). In Arkansas, New Mexico, South Dakota, Virginia, and Wisconsin, the definition of telemedicine has been extended to include voice-only services.
Congressmen have also expanded the treatments that Medicaid covers through telemedicine. At Arkansas, patients are now eligible for a refund for speech-language pathology services performed in physiotherapy, occupational therapy, and distance medicine. Treatment services via electronic communications have been eligible for Medicaid reimbursement in non-rural areas of South Dakota and Minnesota.
Finally, Pennsylvania has recently expanded reimbursement for eligible services within the scope of the provider’s business. All of these states exemplify the steps in the right direction to extend the benefits of telemedicine to everyone who can benefit from them.
About the author: David Nunnally is a Research Assistant at Connected Nation. In this position, he engages in data management, produces research artifacts, and analyzes quantitative data for reports and presentations. For more information on Connected Nation, please visit connectednation.org.
..