New methods may help diagnose Alzheimer’s disease before symptoms appear
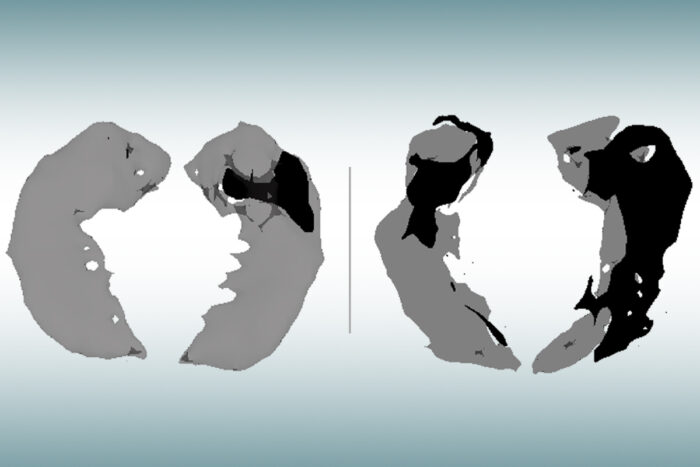
MRI scans of the hippocampus, the memory center of the brains of elderly people with no signs of cognitive decline (left) and people of the same age with mild Alzheimer’s disease (right), show where healthy brain cells are. Lost (dark area) analyzed in. A new study from Washington University in St. Louis’ School of Medicine shows that this new MRI approach can identify brain cell damage in people in the early stages of Alzheimer’s disease before traditional MRI scans show tissue contractions. I am.
Alzheimer’s disease is usually diagnosed based on symptoms such as when a person shows signs of memory loss or difficulty thinking. So far, MRI brain scans have not been proven to be useful for early diagnosis in clinical practice. Such scans can reveal signs of contraction of the brain due to Alzheimer’s disease, but only in the second half of the course of the disease, after the brain is severely damaged and most people are diagnosed by other means. , The signs will be unmistakable.
However, a new study from Washington University in St. Louis found that mathematical analysis of data from the new MRI approach showed the brains of people in the early stages of Alzheimer’s disease, before traditional MRI scans showed tissue contractions. It has been shown to be able to identify cell damage. Cognitive symptoms occur.
“This could be a new way to use MRI to diagnose people with Alzheimer’s disease before symptoms appear,” said Dmitry, a senior author of the Department of Radiology at the University’s Malincrot Radiology Institute.・ Dr. Yabronski said. “This technology takes only 6 minutes to acquire data and can be implemented in MRI scanners already used worldwide for patient diagnosis and clinical trials.”
This study, published in the Journal of Alzheimer’s Disease, relies on a new quantitative gradient echo (qGRE) MRI technique developed in the Yablonskiy lab to show areas of the brain that have failed due to the loss of healthy neurons.
“Using this technique in patients with Alzheimer’s disease, we found a region of the brain that looked normal on traditional MRI but dark on qGRE images, due to significant neurodegenerative disease,” said the Department of Radiology. Said Dr. Satya VVN Kothapalli, Staff Scientist at. The author of the study. “We call them” dark matter. ” “
While traditional MRI can show where the volume of the damaged area of the brain has decreased, qGRE technology goes one step further and detects the loss of neurons that precedes brain contraction and cognitive decline. ..
Alzheimer’s disease progresses slowly for over 20 years before symptoms appear. First, the brain protein amyloid beta accumulates in the senile spots of the brain, and then another brain protein, tau, coalesces and becomes entangled, causing neurons to begin to die. Finally, tissue atrophy becomes visible on MRI brain scans, causing cognitive symptoms. People in the early stages of the disease can be identified by amyloid-PET brain scans or by testing for amyloid in the blood or cerebrospinal fluid that surrounds the brain and spinal cord, but such tests provide information about nerve damage. I will not.
The study enrolled 70 people aged 60-90 years recruited through Charles F. and the Joan Knight Alzheimer’s Disease Research Center (Night ADRC). Participants completed extensive clinical and cognitive tests to assess the level of cognitive impairment. Participant groups included people without cognitive impairment and those with very mild, mild, or moderate disabilities.
Each participant underwent either a PET brain scan or a spinal puncture to measure the amount of amyloid plaques in the brain. They also underwent an MRI brain scan.
Researchers applied qGRE MRI technology to scan the hippocampus, the center of memory of the brain, and one of the earliest affected areas of the brain in Alzheimer’s disease. The results showed that the hippocampus often contained viable tissue sections with dark matter dead zones lacking relatively conserved neurons and substantially healthy neurons.
These dark matter areas were present in people who were positive for amyloid but had not yet experienced symptoms and grew larger as the disease progressed. Compared to traditional MRI measurements of cerebral atrophy, dark matter biomarkers correlated much better with individual cognitive scores for very mild to moderate dementia.
This study builds on and supports findings from a study of Alzheimer’s disease conducted at the University of Washington when Alzheimer’s disease was formally diagnosed only by autopsy over 20 years ago.
In 2001, John C. Morris, MD, Harvey A., and Drismae Hacker, a prominent professor of neurology and director of Knight ADRC, led a study examining the brain tissue of deceased patients with Alzheimer’s disease and injured. Brain areas lose healthy neurons long before the disease causes a significant loss of brain volume in these areas.
Later, in the early 2000s, Tammier LS Benzinger, MD, PhD, a professor of radiology and neurosurgery and director of imaging research at Knight ADRC, pioneered the Mallinckrodt Institute of Radiology using PET brain scans targeting amyloid. Was one of the people. Beta as a tool for detecting Alzheimer’s disease.
In a current study, also co-authored by Morris and Benzinger, researchers used non-invasive qGRE MRI techniques in living patients to record the same association between neuronal loss and symptoms of Alzheimer’s disease. did.
The research team collaborated with co-author Richard Perrin, an associate professor of pathology and immunology, to examine this relationship under a microscope by examining the brain tissue donated after the deaths of study participants. confirmed. Postmortem examination showed that hippocampal neuronal loss actually outweighed tissue volume loss, and these changes were well reflected in dark matter MRI measurements.
Yablonskiy et al. Have low-cost, easily accessible testing for Alzheimer’s disease instead of the expensive PET brain scans and invasive spinal punctures currently used in research environments to assess the presence and progression of Alzheimer’s disease. He is one of the many researchers who are pursuing.
Such tests, especially those that can identify people in the very early stages of the disease, provide significant support for Alzheimer’s disease research and significantly reduce the cost and time required to screen patients for clinical trials. And spur the development of new treatments.
Alzheimer’s disease researchers continue to treat the disease with medication, but most people rely on finding ways to prevent brain damage and early detection before the late stages of Alzheimer’s disease. Agree.
PET scans and spinal punctures continue to play important roles in the study of Alzheimer’s disease, but both have limitations and cannot be widely used as a screening tool for early signs of the disease.
PET brain scans are still the gold standard for detecting signs of Alzheimer’s disease, but machines are expensive, rarely available for routine patient diagnosis, and clinical screening is less prevalent. PET scans also require the injection of a radiotracer for brain imaging.
As Alzheimer’s disease progresses, it can be detected by testing tau protein in the cerebrospinal fluid, but sampling is highly invasive to use as a general screening tool, especially for asymptomatic individuals. Need a spinal puncture that may be too much.
Another promising option for Alzheimer’s disease screening, also under development at the University of Washington, is non-invasive and comparative, which has proven to be very accurate in detecting early signs of Alzheimer’s disease. It is a cheap blood test. Recently, commercial versions of blood tests have become available to doctors in the United States and Europe, but they are not yet covered by health insurance.
Although each test approach has its own strengths and weaknesses, qGRE MRI technology is based on MRI technology that is widely available around the world, is non-invasive, and can be performed without the use of a radiotracer, so it is early. You may be ready to hire.
“Our qGRE test offers great potential as an early diagnostic tool for the preclinical stage of Alzheimer’s disease and thus provides a large window for therapeutic intervention,” said Yablonskiy. “It also has great potential as a non-invasive MRI technique available in traditional clinical settings for the extensive screening required to involve people with early-stage Alzheimer’s disease in clinical drug trials.”
